Background: Genetic alterations are increasingly being recognized to play an important role in both diagnosis and prognosis of MDS. In general, SF3B1 mutated MDS is known to have favorable outcomes whereas those with mutated TP53 have dismal survivals. However, it is unclear if the impact of these mutations applies to all subtypes of MDS including del(5q), a unique entity that is known for its sensitivity to lenalidomide and better prognosis. A prior study suggests TP53 mutations are associated with worse outcomes in del(5q) MDS (Jadersten et al. 2011), but a more recent study did not find this association and instead they showed SF3B1 mutants (MT) conferred shorter survival compared to wild-type (WT) (Meggendorfer et al. 2017). Herein, we describe our experience of del(5q) MDS patients and assess the prognostic impact of somatic mutations in this population.
Methods: We retrospectively reviewed our database of 132 patients with del(5q) MDS who were treated at the Moffitt Cancer Center from 2001 to 2019. Sixty-three patients had molecular data available for analysis. Fisher's exact test of independence was used to determine significance for categorical variables. Univariate and multivariate analyses were conducted using log-rank and Cox regression, respectively. Kaplan-Meier analysis with log-rank test was used to estimate survival outcomes.
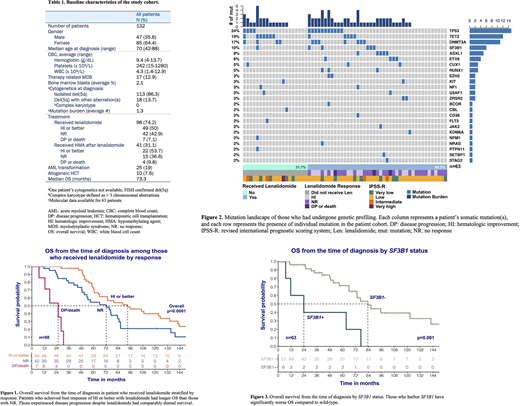
Results: A total of 132 patients (47M/85F) with a median age of 70 at diagnosis were included in this analysis (Table 1). The majority had isolated del(5q) (86.3%) and the remaining with del(5q) plus other aberration(s) but not meeting criteria as complex cytogenetics. Among patients who received lenalidomide (n=98), 50%, 42.9%, and 7.1% achieved hematologic improvement (HI) or better, no response (NR), and disease progression (DP)/death with a median overall survival (OS) of 93.2, 72.4, and 25.6 months from the time of diagnosis, respectively (p<0.0001) (Figure 1). The median OS of the entire cohort was 73.3 months (median follow-up of 131.3 months), and OS from the time patients stopped lenalidomide was only 26 months.
Of the 63 patients with molecular data available, 23.8% were found to have TP53 mutations with a median variant allele frequency (VAF) of 20.4% and 10% SF3B1 MT (median VAF 38.9%). Other common mutations include TET2 (19%) and DNMT3A (17%) as shown in Figure 2. Interestingly, TP53 status did not impact OS (MT 86.4 vs. WT 73.3 months; p=0.72), but those with SF3B1 mutations had a significantly shorter median OS compared to WT (23.9 vs. 83.5 months; p=0.001) (Figure 3). When test for effects of multiple genes had on survival, no combinations were found to be predictive. Univariate analysis showed lenalidomide response significantly impacted OS (HI compared to NR: HR 0.19, 95% CI: 0.05-0.68, p=0.005). Multivariate regression confirmed lenalidomide response and SF3B1 status are independently associated with outcomes.
Conclusions:SF3B1 mutations, typically correlate with favorable risk in MDS, are associated with significantly worse prognosis compared to WT in patients with del(5q) MDS. On the contrary, there was no significant difference in OS in patients with TP53 MT vs. TP53 WT. A substantial portion of patients benefited from lenalidomide; however, after lenalidomide failure survivals were limited. Despite the known overall associations between MDS and mutations such as SF3B1 and TP53, our data suggests the del(5q) subset behaves differently which adds to the heterogeneity of the disease. Further studies are needed to clarify the impact of treatments and somatic mutations on outcomes.
Sallman:Agios, Bristol Myers Squibb, Celyad Oncology, Incyte, Intellia Therapeutics, Kite Pharma, Novartis, Syndax: Consultancy; Celgene, Jazz Pharma: Research Funding. Padron:Novartis: Honoraria; Incyte: Research Funding; Kura: Research Funding; BMS: Research Funding. Lancet:Abbvie: Consultancy; Agios Pharmaceuticals: Consultancy, Honoraria; Astellas Pharma: Consultancy; Celgene: Consultancy, Research Funding; Daiichi Sankyo: Consultancy; ElevateBio Management: Consultancy; Jazz Pharmaceuticals: Consultancy; Pfizer: Consultancy. Komrokji:BMS: Honoraria, Speakers Bureau; Agios: Speakers Bureau; Abbvie: Honoraria; Incyte: Honoraria; Acceleron: Honoraria; Novartis: Honoraria; Jazz: Honoraria, Speakers Bureau; Geron: Honoraria.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal